Overview
The healthcare-associated infection (HAI) component of CEIP engages a network of local health jurisdictions, local hospitals, and academic medical center partners to help answer critical questions about emerging HAI threats, advanced infection tracking methods, and antibiotic resistance in the United States. When combined with HAI data gathered by other EIPs, this information will play a key role in shaping future policies and recommendations targeting HAI prevention.
Objectives:
- Describe the epidemiology of HAI infections
- Obtain estimates of incidence and trends of incidence over time
- Describe new populations at risk
- Provide linked epidemiology and microbiology data on HAI infections to inform prevention approaches
- Characterize specific serotypes causing disease
Tweets from the Society for Healthcare Epidemiology of America
Tweets by @SHEA_Epi
Current Surveillance Projects
- Clostridium difficile infection (CDI) surveillance in San Francisco County
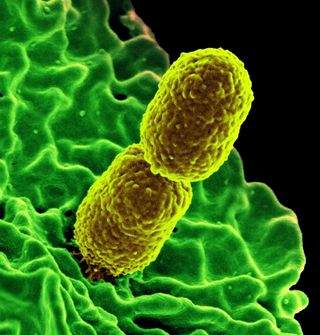
- Invasive staphylococcus aureus (iSA) surveillance in San Francisco, Contra Costa, and Alameda counties
- Candidemia Surveillance in Alameda County
- Multi-Site Gram-Negative Surveillance Initiative (MuGSI) in San Francisco, Contra Costa and Alameda counties which includes Carbapenem-Resistant Enterobacterales (CRE) and Invasive Escherichia coli (iEC) surveillance
Click on project links above for publications.
HAICViz allows you to analyze and visualize data for HAIC surveillance, including Candida bloodstream infections, Clostridioides difficile infections, Staphylococcus aureus infections and case data collected through the Multi-site Gram-negative Surveillance Initiative. Depending on the pathogen, you can look at certain types of data, including: number of case counts and deaths; case and death rates; strain types; syndromes; and antimicrobial resistance.
Completed Projects
I. Healthcare-associated Infections and Antibiotic Use Prevalence Survey
A point prevalence survey conducted on a single day at participating healthcare facilities. The primary objectives of the HAI/antimicrobial use prevalence survey effort are to:
- estimate HAI prevalence in a large sample of inpatients in US acute healthcare facilities
- determine the distribution of HAI by pathogen (including antimicrobial-resistant pathogens) and major infection site
- estimate the prevalence and describe the rationale for antimicrobial use in a large sample of inpatients in US acute healthcare facilities.
Phase 1—Conducted at hospitals in one US city (non-EIP site).
Phase 2—The survey was conducted in all 10 EIP states. 2,015 patients admitted to acute care healthcare facilities were surveyed at 22 acute care facilities. Published results.
Phase 3—The survey was conducted in the 10 EIP states. 11,282 patients admitted to acute care healthcare facilities were surveyed at 183 acute care facilities.
Phase 3 Published results—
- Point Prevalence Survey of Antimicrobial Use in U.S. Acute Care Hospitals. Shelley Magill, Laura McAllister, Melinda Neuhauser, et al. Oral Presentation Session 37, abstract 114 presented at: ID Week 2012. 1st Annual Joint Meeting of ISDA, SHEA, HIVMA, and PIDS; 2012 Oct 16-21; San Diego, CA.
- Prevalence of antimicrobial use in US acute care hospitals, May-September 2011. Magill, S, et. al. JAMA. 2014 Oct 8;312(14):1438-46. doi: 10.1001/jama.2014.12923
- Multistate Point-Prevalence Survey of Health Care–Associated Infections. Magill SS, Edwards JR, Bamberg W, et al.. N Engl J Med 2014;370:1198-208.
Phase 4—The survey was conducted at all sites in the EIP network in 2015. Overall, 12,299 patients in 199 acute care hospitals in 10 EIP states were included in the survey.
Phase 4 Published results—
- Assessment of the Appropriateness of Antimicrobial Use in US Hospitals. Magill, S, et. al. JAMA Netw Open. 2021 Mar 1;4(3):e212007. doi: 0.1001/jamanetworkopen.2021.2007.
- Antimicrobial Use in US Hospitals: Comparison of Results From Emerging Infections Program Prevalence Surveys, 2015 and 2011. Magill SS, O’Leary E, Ray SM, et al. Clin Infect Dis. 2021;72(10):1784-1792. doi:10.1093/cid/ciaa373
- Changes in Prevalence of Health Care-Associated Infections in U.S. Hospitals. Magill SS, O’Leary E, Janelle SJ, et al. N Engl J Med. 2018;379(18):1732-1744. doi:10.1056/NEJMoa1801550
Phase 5—The survey was conducted in 10 EIP states in 2023. Analyses in progress.
II. Emerging Infections Program (EIP) Evaluating SARS-CoV-2 Vaccine Effectiveness Among Health Care Personnel (HCP) During Early Phase Vaccination
This project was conducted to evaluate the effectiveness of the SARS-CoV-2 vaccine in:
- Preventing laboratory confirmed symptomatic COVID-19 among HCP;
- Preventing severe disease among HCP with laboratory confirmed symptomatic COVID-19;
- Comparing between HCP age groups, comorbidities, job categories, and clinical practice settings;
- Comparing between vaccine products available.
Trained staff conducted interviews of healthcare workers that tested both positive and negative for SARS-CoV-2 in 10 EIP sites and other CDC programs nationwide. Medical records and vaccine registry information was additionally reviewed for data verification. A case-control study method was implemented and analyzed to inform real-time decisions regarding vaccine recommendations and to lay the foundation for further research.
Publications
- Vaccine Effectiveness Among Healthcare Personnel Study Team (2021). Interim Estimates of Vaccine Effectiveness of Pfizer-BioNTech and Moderna COVID-19 Vaccines Among Health Care Personnel – 33 U.S. Sites, January-March 2021. Pilishvili, T., Fleming-Dutra, K. E., Farrar, J. L., Gierke, R., Mohr, N. M., Talan, D. A., Krishnadasan, A., Harland, K. K., Smithline, H. A., Hou, P. C., Lee, L. C., Lim, S. C., Moran, G. J., Krebs, E., Steele, M., Beiser, D. G., Faine, B., Haran, J. P., Nandi, U., Schrading, W. A. MMWR. Morbidity and mortality weekly report, 70(20), 753–758. https://doi.org/10.15585/mmwr.mm7020e2
- Vaccine Effectiveness among Healthcare Personnel Study Team (2021). Effectiveness of mRNA Covid-19 Vaccine among U.S. Health Care Personnel. Pilishvili, T., Gierke, R., Fleming-Dutra, K. E., Farrar, J. L., Mohr, N. M., Talan, D. A., Krishnadasan, A., Harland, K. K., Smithline, H. A., Hou, P. C., Lee, L. C., Lim, S. C., Moran, G. J., Krebs, E., Steele, M. T., Beiser, D. G., Faine, B., Haran, J. P., Nandi, U., Schrading, W. A. The New England journal of medicine, 385(25), e90. https://doi.org/10.1056/NEJMoa2106599
- Vaccine Effectiveness among Healthcare Personnel Study Team (2024). Effectiveness of a bivalent mRNA vaccine dose against symptomatic SARS-CoV-2 infection among U.S. Healthcare personnel, September 2022-May 2023. Plumb, I. D., Briggs Hagen, M., Wiegand, R., Dumyati, G., Myers, C., Harland, K. K., Krishnadasan, A., James Gist, J., Abedi, G., Fleming-Dutra, K. E., Chea, N., Lee, J. E., Kellogg, M., Edmundson, A., Britton, A., Wilson, L. E., Lovett, S. A., Ocampo, V., Markus, T. M., Smithline, H. A. Vaccine, 42(10), 2543–2552. https://doi.org/10.1016/j.vaccine.2023.10.072
III. The Emerging Infections Program (EIP) Project to Address COVID-19 Among Healthcare Workers identified risk factors and characteristics of workers who tested positive for SARS-CoV-2.
This project was conducted to address COVID-19 among healthcare workers aimed to assess the:
- Characteristics of healthcare workers with positive tests for SARS-CoV-2, including demographics, role in healthcare delivery, clinical activities, and personal protective equipment (PPE) use.
- Potential risk or protective factors.
To collect this information, trained professionals conducted surveillance and interviewed healthcare workers who tested positive for SARS-CoV-2 in 10 EIP sites between 2020-2021. Healthcare worker interviews concluded December 31, 2021.
Publications
- Practices and activities among healthcare personnel with severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infection working in different healthcare settings—ten Emerging Infections Program sites, April–November 2020. Chea, N, et. al. | Infection Control & Hospital Epidemiology , Volume 43 , Issue 8 , August 2022 , pp. 1058 – 1062. DOI: https://doi.org/10.1017/ice.2021.262
- Risk Factors for SARS-CoV-2 Infection Among US Healthcare Personnel, May–December 2020 – Volume 28, Number 1—January 2022 – Emerging Infectious Diseases journal – CDC
- Residential social vulnerability among healthcare personnel with and without severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infection in Five US states, May–December 2020 | Zoltorzynska, M, et. al | ICHE Volume 45 , Issue 1 , January 2024 , pp. 82 – 88. DOI: https://doi.org/10.1017/ice.2023.131
1. NHSN Denominator Simplification Project – [Published March 2013]
An HAI denominator data collection validation and simplification project in selected acute healthcare facilities (hospitals) was conducted at 10 EIP sites. The results of this project will be used to assess the feasibility and accuracy of using a simplified method for ascertaining HAI denominator data for the National Healthcare Safety Network (NHSN) and will be used to determine how to modify current methodology for NHSN denominator data collection. The primary purpose of the project was to evaluate a simplified, less resource-intense method for obtaining device-days data (compared to current manual data collection practices) to determine if sampling methods can successfully be implemented to collect denominator data and can generate estimates of device-days that are acceptable for HAI surveillance purposes. The primary objectives were to:
- retrospectively assess the feasibility of using sampling methods to obtain estimates of central line-days by analyzing existing data on patient-days and device-days data collected from a large number and variety of inpatient units (both ICU and non-ICU) within acute healthcare facilities
- prospectively assess the feasibility of implementing the use of sampling methods to collect patient-days and central line-days denominator data
- validate estimates of central line-days derived from denominator data collected using sampling methodology against data collected using current denominator data collection practices, and to determine if estimates of central line-days and central line-associated bloodstream infection (CLABSI) rates generated are suitable for the purposes of conducting HAI surveillance and reporting data to NHSN
2. Antibiotic Appropriate Use (Pilot)
Pilot assessment to characterize the indications and documentation related to prescribing select antimicrobial agents to patients in short-stay acute care hospitals identified during the 2011 Phase 3 HAI/antimicrobial use prevalence survey. The primary objectives of this pilot are to:
- test the methods of assessing appropriate prescribing for a full scale evaluation at all eligible facilities in 2013
- determine the proportion of inappropriate antimicrobial use
- inform an independent effort by CDC to create freely available antimicrobial use assessment audit tools for healthcare personnel to utilize in practice improvement initiatives at their hospitals[JN2]
Publications
For additional publications click on project links above for publications.
Multistate Point-Prevalence Survey of Health Care–Associated Infections. Magill SS, Edwards JR, Bamberg W, et al. N Engl J Med 2014;370:1198-208.
CDC Vital Signs Making Health Care Safer, Antibiotic Rx in Hospitals: Proceed with Caution, March 2014
Evaluating the accuracy of sampling to estimate central line–days: simplification of the National Healthcare Safety Network surveillance methods. Thompson ND, Edwards JR, Bamberg W, Beldavs Z, Dumyati G, Godine D, Maloney M, Kainer M, Ray S; Thompson D, Wilson L, Magill SS. Infect Control Hosp Epidemiol 2013; 34(3):221-228.
HAI and antimicrobial use prevalence survey phase 3: point prevalence survey of antimicrobial use in US acute care hospitals. Magill S, McAllister L, Neuhauser M, et al. Oral Presentation Session 37, abstract 114 presented at: ID Week 2012. 1st Annual Joint Meeting of ISDA, SHEA, HIVMA, and PIDS; 2012 Oct 16-21; San Diego, CA.
HAI and antimicrobial use prevalence survey phase 2: preliminary results of a healthcare-associated infection and antimicrobial use prevalence survey in 22 US acute care hospitals. Magill S, McAllister L, Allen-Bridson K, et al. Abstract. SHEA 2011 April 1-4; Dallas, TX.
Comparison of the Risk of Recurrent Clostridioides Difficile Infections Among Patients in 2018 Versus 2013 Guh, AY, Yi SH, Baggs J, Winston L, Parker E, Johnston H, Basiliere E, Olson D, Fridkin SK, Mehta N, Wilson L, Perlmutter R, Holzbauer SM, D’Heilly P, Phipps EC, Flores KG, Dumyati GK, Hatwar T, Pierce R, Ocampo VL, Wilson CD, Watkins JJ, Korhonen L, Paulick A, Adamczyk M, Gerding DN, Reddy SC., Open Forum Infectious Diseases, Volume 9, Issue 9, September 2022, ofac422, https://doi.org/10.1093/ofid/ofac422
Trends in Incidence of Methicillin-resistant Staphylococcus aureus Bloodstream Infections Differ by Strain Type and Healthcare Exposure, United States, 2005-2013. See I, Mu Y, Albrecht V, Karlsson M, Dumyati G, Hardy DJ, Koeck M, Lynfield R, Nadle J, Ray SM, Schaffner W, Kallen AJ. Clin Infect Dis. 2020 Jan 1;70(1):19-25. https://doi.org/10.1093/cid/ciz158.PMID: 30801635
The Landscape of Candidemia During the Coronavirus Disease 2019 (COVID-19) Pandemic. Emma E. Seagle, Brendan R. Jackson,Shawn R. Lockhart, Ourania Georgacopoulos, Natalie S. Nunnally, Jeremy Roland, Devra M. Barter, Helen L. Johnston, Christopher A. Czaja, Hazal Kayalioglu, Paula Clogher, Andrew Revis, Monica M. FarleyLee H. Harrison,Sarah Shrum Davis, Erin C. Phipps, Brenda L. Tesini, William Schaffner, Tiffanie M. Markus, and Meghan M. Lyman; Clinical Infectious Diseases, Volume 74, Issue 5, 1 March 2022, Pages 802–811, https://doi.org/10.1093/cid/ciab562
Contact
For questions about HAI surveillance and HAI projects please contact Erin Parker, MPH.
Erin Parker, MPH
HAIC Project Coordinator
haic@ceip.us[EP4]
More Healthcare-Associated Infections—Community Interface (HAIC[EP5] )
