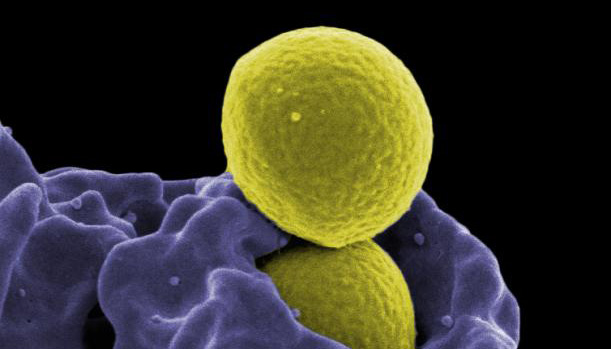
Staphylococcus aureus
Credit – NIAID_Flickr Photostream http://www.flickr.com/photos/niaid/6830921049/
Overview
CEIP conducts surveillance for invasive SA through Healthcare-associated Infections surveillance. For each case of invasive disease in the study population, CEIP generates a case report with basic demographic information.
Objectives
- Evaluate changes in national incidence estimates of hospital-onset (HO), healthcare-associated community-onset (HACO), and community-associated (CA) invasive infections with SA
- Identify new populations at risk for invasive SA disease
- Describe the molecular and microbiologic characteristics of hospital-onset (HO), healthcare-associated community-onset (HACO) and community-associated (CA) SA isolates.
Main Components
The main components of SA surveillance are active laboratory-based surveillance and transmit data to CDC.
Surveillance
Case Definition
A case of invasive SA disease is defined as isolation of SA from a normally sterile site in a resident of the three-county catchment area. This includes both Methicillin-resistant Staphylococcus aureus (MRSA) and Methicillin-sensitive Staphylococcus aureus(MSSA). Normally sterile sites include: blood, cerebrospinal fluid, pleural fluid, peritoneal fluid, pericardial fluid, surgical aspirate, bone, or joint fluid.
Case categorization:
SA cases will be categorized into one of three epidemiologic classes; hospital-onset, healthcare-associated community onset, or community-associated.
A case will be classified as hospital-onset (HO) if the invasive SA culture was collected > 3 calendar days after hospital admission (admit = day 1).
A case will be classified as healthcare-associated community-onset (HACO) if the invasive SA culture was collected ≤ 3 days after hospital admission or as an outpatient, and one or more of the following is documented in the medical record:
- a history of overnight stay in a short- or long-term acute care hospital, surgery, dialysis, or residence in a long-term care facility in the year prior to initial culture; and/or
- a central vascular catheter in place ≤ 2 calendar days prior to the collection of the index culture.
If none of the above criteria are met, the case will be classified as community-associated. Additional information will be abstracted from the chart for each invasive SA disease patient as described below
Data Overview
Data from laboratory line lists and case report forms will be entered into a Microsoft Access or RedCap database (depending on the site’s database preferences); CDC will provide an Access data entry screen to each participating EIP site.
Yearly surveillance reports for pathogens under surveillance are available in PDF format at CDC’s ABCs Surveillance Reports site.
Publications
Kelly A Jackson, Runa H Gokhale, Joelle Nadle, Susan M Ray, Ghinwa Dumyati, William Schaffner, David C Ham, Shelley S Magill, Ruth Lynfield, Isaac See, Public Health Importance of Invasive Methicillin-sensitive Staphylococcus aureus Infections: Surveillance in 8 US Counties, 2016, Clinical Infectious Diseases, Volume 70, Issue 6, 15 March 2020, Pages 1021–1028, https://doi.org/10.1093/cid/ciz323–
Isaac See, Yi Mu, Valerie Albrecht, Maria Karlsson, Ghinwa Dumyati, Dwight J Hardy, Mackenzie Koeck, Ruth Lynfield, Joelle Nadle, Susan M Ray, William Schaffner, Alexander J Kallen. Trends in Incidence of Methicillin-resistant Staphylococcus aureus Bloodstream Infections Differ by Strain Type and Healthcare Exposure, United States, 2005–2013. https://academic.oup.com/cid/article/70/1/19/5364550
Nicole Gualandi, RN, MS/MPH Yi Mu, PhD Wendy M Bamberg, MD Ghinwa Dumyati, MD Lee H Harrison, MD Lindsey Lesher, MPH Joelle Nadle, MPH Sue Petit, MPH Susan M Ray, MD William Schaffner, MD John Townes, MD Mariana McDonald, DrPH Isaac See, MD. Racial Disparities in Invasive Methicillin-Resistant Staphylococcus aureus Infections, 2005-2014. Clin Infect Dis. April 2018. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciy277/4961420
Isaac See, Paul Wesson, Nicole Gualandi, Ghinwa Dumyati, Lee H. Harrison, Lindsey Lesher, Joelle Nadle, Susan Petit, Claire Reisenauer, William Schaffner, Amy Tunali, Yi Mu, and Jennifer Ahern. Socioeconomic Factors Explain Racial Disparities in Invasive Community-Associated Methicillin-Resistant Staphylococcus aureus Disease Rates. Clin Infect Dis. 2017:64. https://academic.oup.com/cid/article/3002713/Socioeconomic
Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison L, Lessa F, Lynfield R, Nadle J, Petit S, Ray S; Schaffner W, Townes J, Fridkin S for the Emerging Infections Program–Active Bacterial Core Surveillance MRSA Surveillance Investigators. National burden of invasive Methicillin-resistent Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 2013; 173(21):1970-1978. doi:10.100 1/jamainternmed.2013.10423.
Links
- EIP’s Active Bacterial Core Surveillance
- MRSA Surveillance
- CDC MRSA Infections
- MRSA Surveillance Reports
- EIP MRSA Publications
Contact
For questions about SA surveillance and projects, please contact:
Joelle Nadle, MPH
Project Coordinator, HAIC
mrsa@ceip.us

